Hospital stays are often a stressful experience for Medicare patients and their families. The worry can intensify when a patient is discharged only to be readmitted to the hospital shortly after. While some readmissions are unavoidable, research indicates significant differences in readmission rates among hospitals. This suggests that the choice of hospital can impact a Medicare patient’s likelihood of being readmitted. For families navigating the complexities of Medicare, understanding hospital readmissions is crucial to ensure the best possible care for their loved ones.
Studies have shown that hospitals can take proactive steps to reduce readmissions. These include providing clear discharge instructions, coordinating care with home health services, and ensuring smooth communication with primary care physicians. For The Medicare Family, these measures translate to better support and a smoother transition home for their loved ones after a hospital stay.
Recognizing the importance of reducing readmissions, Medicare has implemented programs like the Hospital Readmission Reduction Program (HRRP). This program financially incentivizes hospitals to lower their readmission rates, aiming to improve patient care and reduce costs. This article will delve into the HRRP, exploring its effects on Medicare patients and hospitals, examining trends in readmission rates, and discussing key considerations for policymakers and, most importantly, for the medicare family.
Key Insights for The Medicare Family
- In 2017, hospitals faced increased Medicare penalties for readmissions, totaling $528 million. While this may seem distant from the patient, these penalties encourage hospitals to improve care quality, directly impacting the medicare family’s experience.
- Encouragingly, for 2017, it’s estimated that 78% of Medicare patient admissions were to hospitals with either no penalty or minimal penalties (less than 1% of Medicare inpatient payments). This means most medicare families are choosing hospitals focused on reducing readmissions.
- Since 2012, national readmission rates for Medicare patients have been declining. This positive trend suggests that hospital initiatives and programs like HRRP are working, leading to fewer readmissions for the medicare family.
- However, it’s important to note that certain hospitals, particularly major teaching hospitals and those serving a large proportion of low-income patients, are more likely to face penalties. For the medicare family, this highlights the importance of understanding hospital quality metrics beyond just location.
What is a Hospital Readmission? Defining it for The Medicare Family
For Medicare purposes, a hospital readmission is defined as a patient being admitted back into a hospital within 30 days of being discharged from a previous hospital stay. This 30-day window applies regardless of which hospital the patient is readmitted to, and it includes readmissions for any medical reason. Medicare uses an “all-cause” definition, meaning any hospital stay within 30 days of discharge counts as a readmission, no matter the cause. This broad definition is used to calculate both national and hospital-specific readmission rates.
It’s important for the medicare family to understand this 30-day window. If a loved one is discharged, closely monitoring their health and ensuring follow-up care within this period is vital to potentially prevent a readmission. Planned hospitalizations, like scheduled procedures, are not counted as readmissions, offering some clarity in complex situations.
Currently, the HRRP focuses on readmissions following hospitalizations for specific conditions: heart attack, heart failure, pneumonia, COPD, elective hip or knee replacement, and CABG. While Medicare tracks overall readmission rates, penalties are specifically tied to these conditions. For the medicare family facing these conditions, understanding readmission risks and focusing on hospitals with strong performance in these areas is particularly relevant.
The Hospital Readmission Reduction Program: How it Impacts The Medicare Family
Established under the Affordable Care Act (ACA), the HRRP penalizes hospitals with high readmission rates for traditional Medicare patients by reducing their Medicare payments. This program, a permanent part of Medicare, applies to most acute care hospitals, excluding specialized facilities like psychiatric or children’s hospitals.
Hospitals with readmission rates exceeding the national average face payment reductions across all Medicare admissions, not just those leading to readmissions. Medicare adjusts for patient demographics and illness severity before comparing hospital rates to the national average. This adjusted rate of “excess” readmissions determines the penalty – higher excess readmissions mean higher penalties. Each year, Medicare publishes hospital-specific penalties, making this information accessible for the medicare family to research and consider when making healthcare decisions.
The maximum penalty started at 1% in 2013, increased to 2% in 2014, and reached its full phase-in of 3% in 2015 (see Table 1). Penalties are calculated using three years of hospital data. For example, 2017 penalties were based on readmissions from July 2012 to June 2015.
| Table 1: The First Five Years of the Hospital Readmission Reduction Program |
|---|
| Year penalties applied |
| Performance (measurement) period |
| Diagnoses of initial hospitalization |
| Penalties: Percentage reduction in base payments on all Medicare inpatient admissions |
| Maximum rate of penalty |
| Average hospital payment adjustment (among all hospitals) |
| Average hospital penalty (among penalized hospitals only) |
| Percent of hospitals penalized |
| Percent of hospitals at max penalty |
| CMS estimate of total penalties |
| NOTES: *Additional types of pneumonia diagnoses added for 2017. Penalties are applied to each hospital in the year shown, based on performance during the preceding 3-year measurement period. Penalties assessed as reductions in base payments on all Medicare inpatient admissions, and do not apply to added payment adjustments, such as graduate medical education payments. Analysis excludes hospitals not subject to HRRP, such as Maryland hospitals and other hospitals not paid under the Medicare Hospital Inpatient Prospective Payment System, such as psychiatric hospitals. COPD: Chronic obstructive pulmonary disease. Estimates of total penalties reflect CMS’s published corrections for 2013 and 2014. CABG: coronary artery bypass grafting. FY: fiscal year. SOURCE: Kaiser Family Foundation analysis of CMS Final Rules and Impact files for the Hospital Inpatient Prospective Payment System. |
Initially, penalties focused on readmissions for heart attack, heart failure, and pneumonia. Over time, COPD and hip/knee replacement were added in 2015, and CABG and expanded pneumonia diagnoses in 2017. This expansion indicates Medicare’s growing focus on reducing readmissions across a wider range of conditions relevant to the medicare family.
Increased Fines in 2017: What it Signifies for The Medicare Family
In 2017, the average penalty across all hospitals was a 0.58% reduction in base Medicare payments. For hospitals penalized, the average reduction was 0.74%, a notable increase from the previous year. This increase led to an estimated total of $528 million in penalties, up from $420 million in 2016. The proportion of hospitals penalized remained relatively stable at around 78-79%.
The primary driver for these increased penalties in 2017 was the inclusion of more medical conditions in the readmission calculations, specifically CABG and expanded pneumonia diagnoses. This expansion, and the increasing average penalties, signals Medicare’s continued emphasis on holding hospitals accountable for readmission rates and incentivizing improved patient care for the medicare family.
It’s important to understand that penalties are based on average hospital performance, not fixed targets. This means that even with national improvements in readmission rates, a certain percentage of hospitals will always be penalized. While this may seem counterintuitive, it’s designed to continuously push hospitals to improve and strive for better-than-average performance in reducing readmissions, ultimately benefiting the medicare family.
Where Medicare Patients Are Receiving Care: Implications for The Medicare Family
Analysis reveals that most Medicare patients are admitted to hospitals with low or no readmission penalties. In 2017, approximately 78% of Medicare patient stays were in hospitals with penalties less than 1% or no penalty at all (Figure 1). This is good news for the medicare family, suggesting that the majority are accessing hospitals that are performing well in readmission reduction. Conversely, about 22% of stays were in hospitals with penalties exceeding 1%, and only around 1% in hospitals facing the maximum 3% penalty.
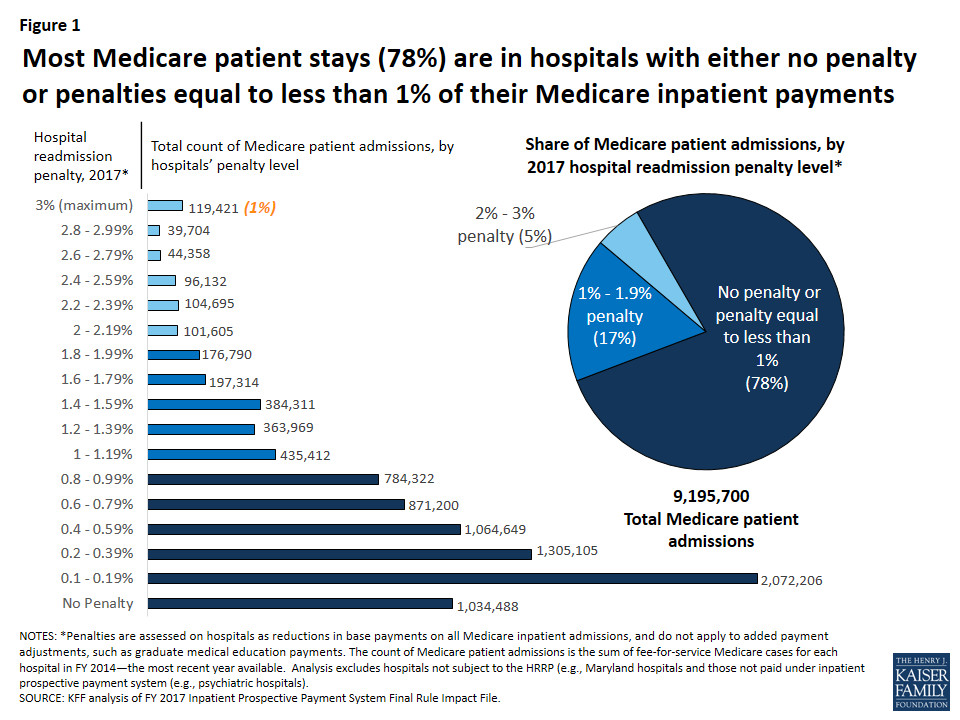 Figure 1: Most Medicare patient stays (78%) are in hospitals with either no penalty or penalties equal to less than 1% of their Medicare inpatient payments
Figure 1: Most Medicare patient stays (78%) are in hospitals with either no penalty or penalties equal to less than 1% of their Medicare inpatient payments
For the medicare family, this data emphasizes the importance of informed hospital selection. While hospital choice can be influenced by location and insurance networks, understanding a hospital’s readmission penalty status can be an additional factor in making decisions about where to seek care.
Hospital Characteristics and Readmission Penalties: What Families Should Consider
Further analysis shows that certain types of hospitals, including major teaching hospitals and those serving higher proportions of low-income patients, are more likely to face penalties and higher penalties (Table 2). This aligns with previous research and highlights potential disparities in healthcare. Major teaching hospitals often function as safety-net hospitals, serving more vulnerable populations.
| Table 2: Variation in penalties by hospital characteristics, 2017 |
|---|
| Hospital type |
| All |
| Rural/urban |
| Urban |
| Rural |
| Teaching status |
| Major teaching |
| Other teaching |
| Nonteaching |
| Size |
| 39% |
| 100-299 beds |
| 300+ beds |
| Proportion of patients who are low-income, Medicare |
| Quartile 1 (Lowest) |
| Quartile 2 |
| Quartile 3 |
| Quartile 4 (Highest) |
| NOTES: The low-income Medicare patient proportion is derived from hospital ratios of Supplemental Security Income (SSI) patient days, with the 4th quartile having the highest ratio of low-income patient days. The percent of hospitals in each group is for 2016. The percent of patient admissions is from based on the March 2015 update of the FY 2014 MedPAR. Analysis excludes hospitals not subject to HRRP because they are not paid under the Medicare Hospital Inpatient Prospective Payment System (e.g., Maryland hospitals, psychiatric hospitals). Penalties assessed as reductions in base payments on all Medicare inpatient admissions, and do not apply to added payment adjustments, such as graduate medical education payments. SOURCE: Kaiser Family Foundation analysis of CMS Final Rules and Impact Files for the Hospital IPPS; CMS SSI calculations are from 2014 claims run out. |
Hospitals with the lowest proportion of low-income patients are least likely to be penalized. Rural hospitals also experience higher penalty rates and average penalties. These variations, consistent over the HRRP’s first five years, suggest systemic factors influencing readmission rates. For the medicare family, especially those in rural areas or with limited resources, understanding these trends can inform their approach to healthcare planning and advocacy.
Declining Readmission Rates: A Positive Trend for The Medicare Family
Medicare has been publicly reporting hospital readmission rates on its Hospital Compare website since 2009, along with other quality and patient satisfaction measures. This website allows the medicare family to compare hospital performance against national averages, identifying hospitals performing “better,” “worse,” or “no different” than the national rate. In addition to condition-specific readmissions, overall Medicare readmission rates are also available.
Analysis of this data reveals a significant trend: readmission rates began to decline in 2012 (Figure 2). This decline, observed across multiple diagnosis categories, coincided with the enactment of the HRRP. This suggests that the program has been effective in prompting hospitals to implement interventions aimed at reducing readmissions, directly benefiting the medicare family by reducing the likelihood of readmission. The Department of Health and Human Services estimates 565,000 fewer Medicare patient readmissions between April 2010 and May 2015, a substantial improvement.
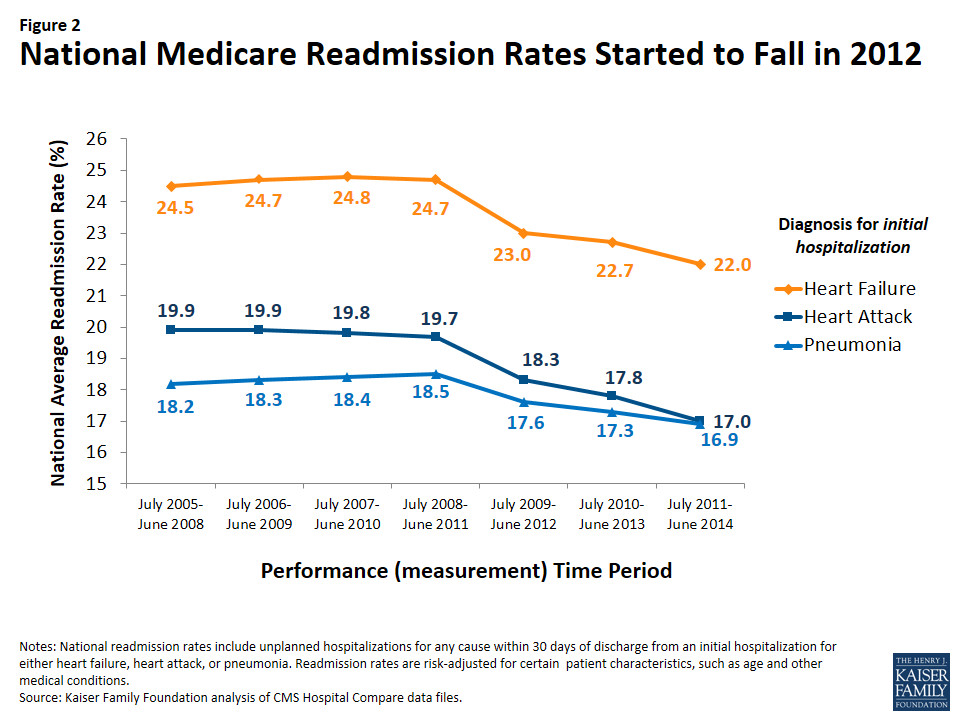 Figure 2: National Medicare Readmission Rates Started to Fall in 2012
Figure 2: National Medicare Readmission Rates Started to Fall in 2012
Despite declining readmission rates, average HRRP penalties have not decreased. This is because penalties are calculated based on relative hospital performance compared to the national average, not fixed targets. While national readmission rates are improving, the HRRP’s structure ensures continued pressure on hospitals to enhance their performance, further driving down readmissions for the medicare family in the long run.
Policy Considerations and The Medicare Family
Policymakers are continuously considering refinements to the HRRP based on feedback from researchers and hospitals. These refinements could impact how hospitals are measured and penalized, indirectly affecting the care received by the medicare family. Some key policy issues include:
- “Moving Goalposts” and Multiple Measures: The HRRP’s penalty calculations are based on comparisons to national averages, creating a “moving goalpost.” As national readmission rates decline, hospitals must continuously improve to avoid penalties. Some argue for fixed targets for all-condition readmission measures to provide hospitals with clearer goals. Others argue that fixed targets might reduce the incentive for continuous improvement. For the medicare family, the debate centers on ensuring sustained improvement in hospital care and reduced readmissions.
Discussion: What This Means for The Medicare Family
This analysis shows that the majority of Medicare patient admissions (78%) are to hospitals with low or no readmission penalties. Considering the stress and difficulties associated with hospital readmissions, it’s reassuring for the medicare family to know that most Medicare beneficiaries are receiving care in hospitals with relatively lower readmission rates. While hospitals with higher penalty rates account for a smaller proportion of stays, higher readmission rates can indicate potential concerns about care quality and discharge planning. Therefore, the medicare family should be aware of hospital readmission performance as one factor in their healthcare choices.
The overall decline in national Medicare readmission rates since 2012 is a positive trend. It suggests that hospital efforts, potentially spurred by the HRRP, are contributing to fewer readmissions. This is likely due to system-wide improvements and a broader focus on readmission reduction across the healthcare system. For the medicare family, this translates to a healthcare system increasingly focused on preventing readmissions and ensuring smoother transitions home after hospital stays.
However, disparities persist. Hospitals serving higher proportions of low-income Medicare patients continue to face higher readmission rates and penalties. Socioeconomic factors can significantly impact a patient’s recovery and access to necessary support services after discharge. Limited access to transportation, home care, and healthy food in lower-income communities can increase readmission risk. Addressing these social determinants of health is crucial to further reduce readmissions and ensure equitable healthcare for all members of the medicare family, regardless of socioeconomic background.
Congress has acknowledged these socioeconomic issues and mandated a new “peer group” method for assessing hospital performance, categorizing hospitals based on their proportion of dually eligible Medicare and Medicaid patients. However, variations in state Medicaid eligibility criteria raise concerns about the fairness and accuracy of this approach. For the medicare family, this highlights the complexity of healthcare policy and the ongoing efforts to refine programs like HRRP to address disparities and improve patient outcomes.
Ultimately, the HRRP’s impact on the medicare family is primarily indirect. By incentivizing hospitals to improve care and reduce preventable readmissions, the program aims to enhance the quality of care for Medicare patients. While some argue that penalties could strain already challenged hospitals, the goal is to drive improvements that benefit patients and the Medicare system as a whole. It’s important to note that hospital penalties do not directly affect a beneficiary’s out-of-pocket expenses, although readmissions themselves can lead to additional costs and burdens for the medicare family.
Looking Ahead: The Future for The Medicare Family and Readmission Reduction
The HRRP and related initiatives have successfully brought attention to the importance of reducing preventable hospital readmissions. Programs like Accountable Care Organizations (ACOs), bundled payment models, and transitional care management are further reinforcing the focus on readmission reduction within Medicare. These programs aim to create a more coordinated and patient-centered healthcare system, which is beneficial for the medicare family.
As more data emerges from these payment and delivery system reforms, a key focus remains on improving care for patients with complex health needs, particularly those with a history of hospitalizations. Continued reductions in preventable readmission rates are a crucial metric for measuring success. Lower readmissions not only contribute to slowing the growth of Medicare spending but also signal improvements in patient care during and after hospital stays, leading to better health outcomes and peace of mind for the medicare family.
Appendix

